By Leila Waid.
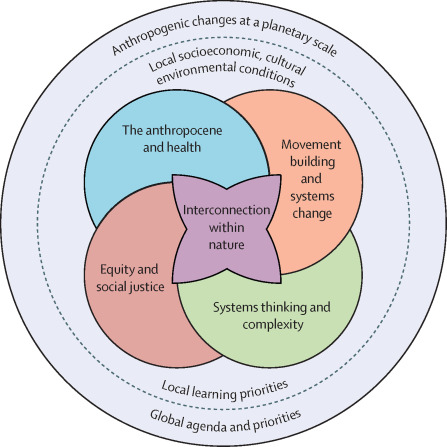
Planetary health is a term used to define how human activity impacts the environment and, in turn, how those environmental changes impact human health. Utilizing a planetary health framework is essential for environmental health organizing because it uses a holistic approach to understanding the world and our place within it. The Planetary Health approach showcases that protecting our environment is not something we should do because it is simply the right thing, but we need to do it for our preservation and well-being.
The air we breathe is littered with pollution from fossil-fuel industries. Even antibiotic resistance, a major emerging public health threat, has connections to air pollution. For example, a study found that PM2.5 (particulates in the air smaller than a strand of hair) contain antibiotic-resistant bacteria. Shockingly, the study found that “the magnitude of the contribution of PM2.5 to aggregate antibiotic resistance is greater than that of antibiotic use.”
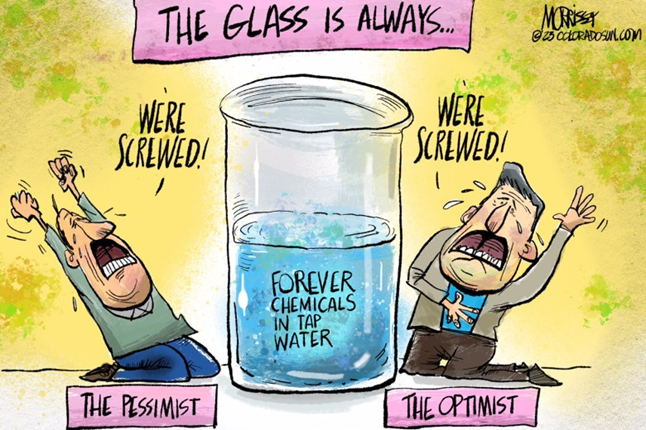
Our waterways are full of plastics and PFAS, a group of forever chemicals that bioaccumulate in the body. The fish we consume are saturated with methylmercury due to humanmade activity, such as coal mining that dumps excess mercury into the waterways. And we keep pumping greenhouse gases into the environment, which causes warming and a disbalance in our delicate climate system. Interestingly, even the knowledge that we are driving the deterioration of the natural world causes stress and other mental health issues – a phenomenon coined “eco-anxiety.” On the other hand, being in nature does wonders for our mental health, such as decreasing anxiety and depression.
So, what can be done? How can we keep our quality of life, with all our modern conveniences, while understanding that profound changes must be made to preserve the ecological world and our health? Two public health experts, Tong and Bambrick, weigh in on this issue in a peer-reviewed article, in which they provide four suggestions.
According to Tong and Bambrick, we first need to address the root cause of climate change globally and utilize different approaches based on regional and national contexts. Second, we must address environmental justice at all levels, from international to hyper-local. Third, we must understand that the entire world is interconnected, and we live in a “global village.” Our air and waterways do not have national boundaries, and the air pollution on one side of the world can eventually reach your backyard. Nowhere was this more apparent than the summer of 2023 on the east coast of the U.S. when the Canadian wildfire plume traveled south and made the air unbearably smoggy. The fourth, and final, suggestion states that we must take collective action at an international level. After all, these are not issues that one individual or country can tackle. Instead, we need to reimagine our way of life that is focused on being connected to our environment, respecting our limited natural resources, and protecting human health.
Planetary health lays out the vicious cycle that modern humans face. We have built our way of life not in tandem with the natural world but in its exclusion. And as a result, we face the health consequences of those choices.